Revitalize Your Chiropractic Practice
In this blog, we’ll explore the important things chiropractic offices should do and remember to set the stage for a year of increased reimbursement and reduced risk.


This Documentation Gap Analysis allows us to evaluate the significant components of your current Documentation program. It should take less than 5 minutes to complete.

Sometimes you need more than a self-service, on-demand program and need an expert to analyze your issues, train the corrections, and help you implement the changes, so they stick

This course explains the significant role chiropractic care can play in the sports industry and how a DC can succeed as a Sports Chiropractor. Start your steps to success here!

The most effective chiropractic OIG compliance programs are scaled according to the size of the practice!
In this blog, we’ll explore the important things chiropractic offices should do and remember to set the stage for a year of increased reimbursement and reduced risk.

Thank you for entrusting us with your needs. Your continued support inspires us to strive for excellence every day. Wishing you and your loved ones a Merry Christmas filled with happiness and blessings. Here's to a fruitful and prosperous 2024!
Good communication will enhance the doctor-patient relationship. Keep your ears open to hear how you can best help your patients.
If you were unable to attend, or would like to watch the "Managing the Insurance Circus: Be the Ringmaster, Not the Act!" Tour again, we’ve made it available for you here:

“As we express our gratitude, we must never forget that the highest appreciation is not to utter words but to live by them.” ~ John…
There comes a point in the doctor-patient relationship when the doctor has done all they can, and it is in everyone’s best interest to refer a patient out to another provider. Your documentation needs to address the referral process since it is an important part of the patient’s story.
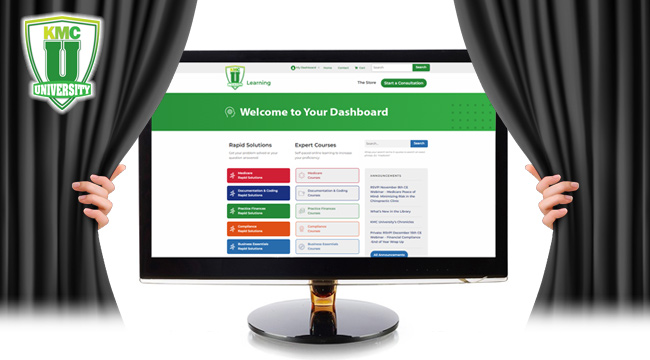
At KMC University or goal is to do all we can to benefit the chiropractic profession. We want to help alleviate many of the burdens you face as a doctor, giving you more time to focus on what truly matters: patient care.
Most providers are unaware of and never look for the red flags in their documentation and coding which could trigger an audit.
SOAP Documentation: Prevent Financial Consequences Many doctors have invested thousands of dollars in an EHR system loaded with templated macros used to create their…
CMS announced, “Patient’s Medicare Beneficiary Identifier (MBI) May Change” due to a recent breach.