What is an ABN and Why Do I Have to Sign It?
If you’re a Medicare patient receiving chiropractic care, you might be asked to sign a form called an Advance Beneficiary Notice, or ABN for short. This form is important because it helps you understand when Medicare won’t cover certain services, like wellness visits or maintenance adjustments.
Let’s break down what this form really means and why your chiropractor is asking for your signature.
What’s an ABN?
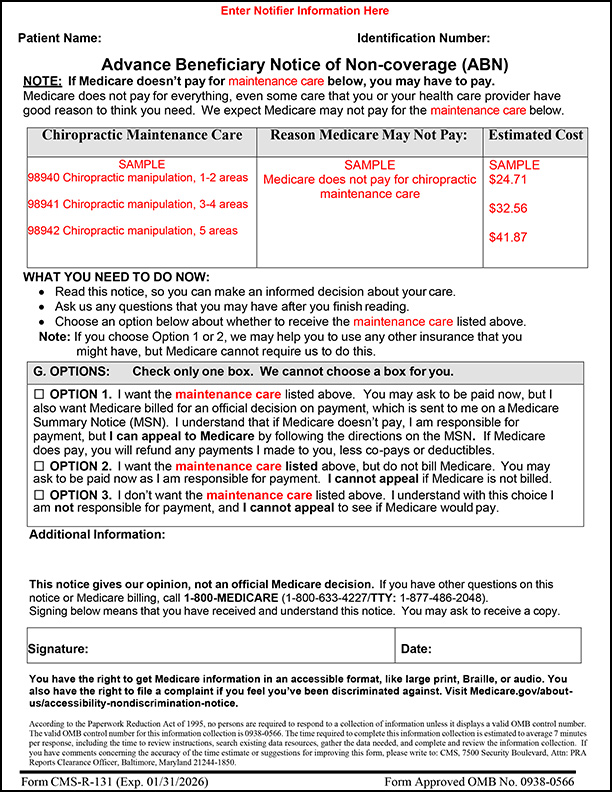
An Advance Beneficiary Notice (ABN) is a form Medicare requires your doctor to provide to you when Medicare won’t cover your chiropractic adjustments. It lets you know what the service is, how much it might cost, and what your options are for proceeding.
Think of it like a heads-up before care is given. It helps you make an informed choice: whether you still want the service knowing you must pay for it yourself.
Why Do I Have to Sign It?
Medicare only pays for chiropractic adjustments (called “CMT services”) when they are medically necessary, usually for active treatment of a specific condition. If your care shifts to wellness or maintenance (ongoing care to keep you feeling good), Medicare doesn’t cover that. The ABN is used in those cases to notify you that:
- Medicare is likely to deny the charge
- You will be responsible for the cost
- You still have the right to choose whether or not to receive the service
Do I Have to Sign One Every Visit?
No. If you’re getting the same type of non-covered care regularly, like a maintenance adjustment once a month, you can sign one ABN that’s good until you may have another condition for which Medicare will begin paying again. Then, when that condition resolves and you begin another period of maintenance care, your doctor will ask you to sign a new one.
What Happens If I Don’t Want to Sign?
You always have the right to say no. If you do not want to receive the non-covered maintenance care, you don’t have to. However, if your doctor is recommending it, it is because it is important to your health. It is your responsibility to understand why your doctor is recommending maintenance care so you can make an informed decision. Be sure to confirm what your out-of-pocket costs will be. If you still do not want the maintenance care, your doctor will note your refusal on the form and give you a copy.
What Are My Options on the ABN?
The ABN gives you three choices:
- Option 1: Yes, I want the service and I want Medicare billed to see the denial. I agree to pay now and will be refunded should Medicare cover it.
- Option 2: Yes, I want the service but don’t want it billed to Medicare. I agree to pay now and understand I will not receive an official denial.
- Option 3: No, I don’t want the service.
Do I Need an ABN for Every Service?
Not necessarily. Medicare never covers services like exams, x-rays, and therapies when performed by a chiropractor. For these, your provider might give you a “voluntary” ABN, or a special notice to let you know you’ll be paying out of pocket. This isn’t required, but it’s a good way to keep things clear.
Anything Else I Should Know?
If you have both Medicare and Medicaid (called “dual-eligible” or “QMB”), there are special rules. You generally cannot be charged your deductible or cost-sharing at the time of service. Medicare-covered services that are denied by both programs may become your responsibility. Your provider can explain how this works and help you understand your rights.

