What is Medical Necessity in Chiropractic Care?
Medical necessity determines whether your chiropractic care qualifies for insurance coverage. While chiropractors diagnose and develop treatment plans for their patients, not all care meets the definition of medical necessity. Insurance companies and other payers use specific criteria to decide what they will cover.
Medically Necessary vs. Clinically Appropriate Care
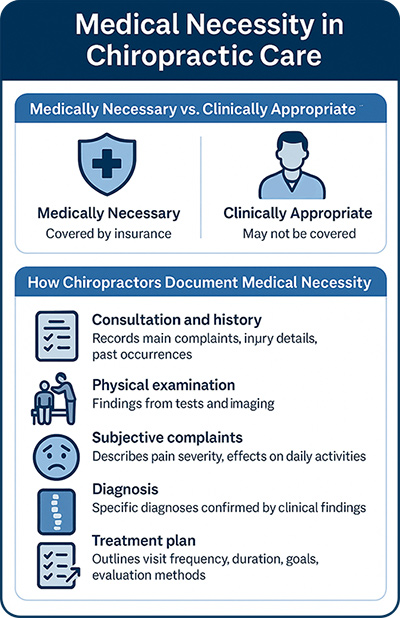 Chiropractic care can be both clinically appropriate and medically necessary, but these terms are not the same. Clinically appropriate care refers to any treatment that your doctor may provide to you. However, insurance companies only cover treatments they classify as medically necessary.
Chiropractic care can be both clinically appropriate and medically necessary, but these terms are not the same. Clinically appropriate care refers to any treatment that your doctor may provide to you. However, insurance companies only cover treatments they classify as medically necessary.
Each insurance provider has different rules. Some follow Medicare guidelines, requiring proof of a spinal subluxation causing a neuromusculoskeletal condition. Others allow coverage based on your chiropractor’s diagnosis and treatment plan. Generally, for care to be medically necessary, you must have a significant health condition with a reasonable expectation of improvement. Your provider proves this necessity through documentation, including your history, exams, daily treatment notes, treatment plan, and imaging when needed.
How Chiropractors Document Medical Necessity
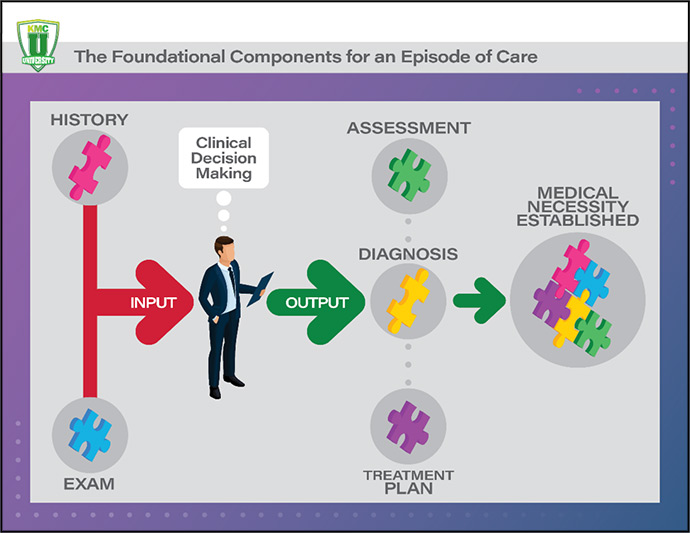
Your chiropractor must document medical necessity from your first visit through the conclusion of your treatment. Each note must align with your diagnosis, treatment, and progress toward recovery. This process, known as episodic care, ensures effective care to regain your functional loss.
Your records may include:
- Consultation and history – Your chiropractor records your main complaints, injury details, and any past occurrences of the issue.
- Physical examination – They document findings from orthopedic and neurological tests, range of motion assessments, and imaging results.
- Subjective complaints – You describe your pain’s severity, what worsens or relieves it, and how it affects daily activities.
- Diagnosis – Chiropractors use specific diagnoses confirmed by clinical findings.
- Treatment plan – The plan outlines visit frequency, duration, goals, and evaluation methods to measure progress.
To prove that treatment remains necessary, your provider reassesses you periodically, measuring improvements and adjusting your care plan as needed.
Challenges in Proving Medical Necessity
Insurance companies set strict guidelines to control costs. Many require pre-authorizations and detailed documentation before approving claims. This process can be frustrating for both chiropractors and patients.
Factors that support claim approval:
- Your condition is likely to improve with chiropractic treatment.
- The recommended treatment matches your diagnosis.
- No contraindications prevent treatment.
- Your provider’s notes show clear progress toward specific health goals.
- You have not yet reached your maximum therapeutic benefit.
Reasons claims may be denied:
- Insufficient documentation supporting the diagnosis.
- Lack of detail about your symptoms and functional limitations.
- A mismatch between the treatment plan and the diagnosis.
- No measurable goals for treatment.
- Extended reliance on passive therapies without progression to active care.
The Role of Your Treatment Plan
Your treatment plan plays a key role in determining medical necessity. Chiropractors assess your condition based on whether it requires short-term care or an extended treatment approach. They categorize treatment needs as:
Incident care – A short-term issue that resolves quickly.
Burst care – A condition requiring moderate treatment over several weeks.
Full episode care – A complex issue needing extended treatment with progressive milestones.
By understanding medical necessity, you can better navigate insurance coverage and ensure you receive the chiropractic care you need.

