Posted by nuclearnetworking on Oct 11, 2018
Swimming in BCBS Therapy Denials? Take a Pro Active Approach
It has been brought to our attention that many providers are experiencing an overwhelming number of Blue Cross and Blue Shield (BCBS) denials for claim items billed with modifiers. The EOBs reflect that the, “modifiers are used inappropriately” or “utilization of modifier is higher than average.” These denials are a result of a new code-editing feature announced to all provider types in a BCBS Newsletter dated August 2017. Although this edit is applied to claims from all provider types, the codes primarily affecting doctors of chiropractic are E/M codes and 97140.
What can you do?
We encourage you not to ignore these denials. Before resubmitting the claims, investigate to determine whether or not the modifiers were properly submitted. For example, modifier -25 should be appended to E/M codes ONLY if performed on the same date as CMT and if “the patient’s condition requires a separately identifiable E/M service beyond the usual pre-service and post service work associated with the procedure.” If you have billed this correctly, you MUST appeal the claim. Send in the proper documentation to show the seperately identifiable E/M service, along with a summary template asking for reconsideration. Theoretically, once they determine that your -25 modifiers are being billed correctly, the denials should stop or the edit should be corrected.
As we’ve worked with doctors on this issue, we have observed the use of modifier-25 on CPT codes other than E/M codes, or worse yet, appended to an E/M code when an E/M is not billed with a CMT. If your practice management system defaults to appending an automatic modifier -25 to each E/M code, this should be corrected immediately. Be sure that your documentation supports a valid reason for performing an E/M in addition to a CMT (e.g., a new condition, new injury, exacerbation, or re-evaluation for treatment plan modification).
If you are appending modifier -59 to CPT code 97140 your documentation must clearly identify a separate body region on which the therapy was applied. Remember this is a claim edit, so it is important that the claim clearly identifies a separate and distinct region. You can do this through the use of diagnosis pointers as shown in Box 24 E and Box 21 (See Fig 1 and Fig. 2). NOTE: confirm whether the carrier you’re billing has adopted the use of the “X” modifiers in lieu of the 59 modifier. That can also be a reason for denial of 97140 with a 59 modifier. Again, be sure to appeal these denials when the billing has been submitted correctly, but denied anyway!
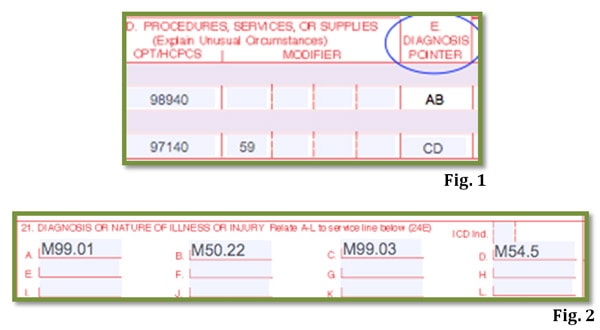
If your practice management software defaults to the same letters (diagnosis pointers) for all lines of service, this, too, should be corrected immediately.
It has been brought to our attention that some consultants are under the impression that CPT changed its position on billing therapy codes 97110-97124 with CMT. This is an inaccurate assumption.
The following was stated in CPT Assistant® May 2010:
| Question: Is it appropriate to report codes 97110-97124, if the procedure were performed at the same region as Chiropractic Manipulative Treatment (CMT)?
Answer: Yes. The physical medicine and rehabilitation procedure codes 97110-97124 codes, represent distinctly separate and unrelated procedures, which are not considered inclusive of CMT as described by codes 98940-98943. Therefore, when the procedure is distinct from the manipulation, it would be appropriate to report codes 97110-97124 in addition to CMT, when performed at the same anatomic site (e.g., separate body regions are not required). Since CPT considers these codes a separate and distinct procedure, appending modifier -59 would not be necessary. Remember modifier -59 alerts the payer that “procedures/services, other than E/M services, that are not normally reported together, but are appropriate under the circumstances” were rendered. In this case, 97110-97124 already are considered distinct by CPT definition. With this in mind, unless the payer requires you to append modifier -59 to the code set 97110-97124 (which is against CPT advice) we recommend that you avoid doing so. Applying modifier-59 to all therapy codes could cause your clinic to fall into the category of ‘overuse’ with the payer. |
CPT Assistant® November 2016 clarified AMA’s stand on procedure code 97140:
| Question: Is it appropriate to report code 97140, Manual therapy techniques (e.g., mobilization/manipulation, manual lymphatic drainage, manual traction), 1 or more regions, each 15 minutes, with modifier 59, Distinct Procedural Service, appended for a separate procedure such as myofascial release, when performed by the same provider at the same session with chiropractic manipulative treatment (CMT), where both procedures are performed to the same spinal region?
Answer: No, modifier 59 indicates that the procedure was provided to a separate anatomical body region. Given the similarity in the two procedures (CMT as compared to procedures described in code 97140), reporting of both procedures to the same body region is not appropriate. The rationale behind disallowing CMT and manual therapy techniques represented by code 97140 to be reported for the same anatomic site is due to overlap of preservice, intraservice, and postservice work that is inherent to both codes. The intraservice overlap occurs as the provider identifies the osseous, articular, and soft tissue restrictions. In addition, both procedures incorporate spinal and peripheral manual joint and soft tissue techniques. Under certain circumstances, it may be appropriate to additionally report CMT/OMT codes in addition to code 97140 if the procedures were performed on separate anatomical regions. In those cases, modifier 59 should be appended (97140-59 to indicate that a distinct procedural service was provided. [Emphasis added] |
Summary
We encourage you and your clinic staff to take a pro-active approach in order to avoid additional denials. You can do this by checking your practice management software for proper appendage of modifier -59 and -25. Double check your diagnosis pointers and confirm that treating doctors are clearly communicating the appropriate CPT code to bill for each diagnosis/condition.
KMC University Library Members
If you think you have crossed your ‘t’s and dotted your ‘I’s yet you are still receiving denials, we encourage you to locate the helpful resources in our 3rd-Party Billing Collections department of the KMC University Library; Classroom 6, Lesson 1 – Appealing Denials. The lesson offers easy-to-use Appeal Template letters that address both 97140 and E/M with CMT. If your clinic needs a refresher on coding and modifiers, visit the Coding Department, Classroom 2, Lesson 3 – Coding Muscle Therapies and Classroom 3, Lesson 1 – Overview of E/M.







Comments on Overwhelmed with Therapy Denials from BCBS?